Alzheimer’s Association and the Centers for Disease Control and Prevention. Alzheimer’s Association. The Healthy Brain Initiative: The Public Health Road Map for State and National Partnerships, 2013–2018. Chicago, IL: Alzheimer’s Association; 2013. http://www.alz.org/publichealth/downloads/2013-RoadMap.pdf. Accessed February 14, 2020.
Alzheimer’s disease research – awareness, education and care (Spring, 2011) • UNC Gillings School of Global Public Health. UNC Gillings School of Global Public Health. 2011 [accessed 2020 Feb 18]. https://sph.unc.edu/cphm/were-racing-ahead-spring-2011/alzheimers-disease-research-awareness-education-and-care-spring-2011/
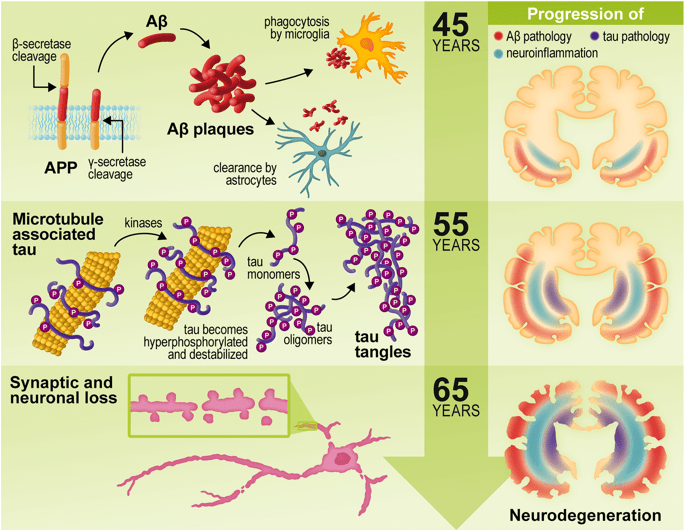
Heneka MT, Carson MJ, Khoury JE, Landreth GE, Brosseron F, Feinstein DL, Jacobs AH, Wyss-Coray T, Vitorica J, Ransohoff RM, et al. Neuroinflammation in Alzheimer’s disease. The Lancet Neurology. 2015 Mar 16 [accessed 2020 Jan 15]. https://www.sciencedirect.com/science/article/pii/S1474442215700165
Insel PS, Hansson O, Mackin RS, Weiner M, Mattsson N. Amyloid pathology in the progression to mild cognitive impairment. Neurobiology of Aging. 2017 Dec 27 [accessed 2020 Jan 22]. https://www.sciencedirect.com/science/article/pii/S019745801730413X
NC State Aging Profile. North Carolina is Aging. North Carolina State Government. 2017 December 1 [accessed 2020 Feb 1]. https://files.nc.gov/ncdhhs/documents/files/NC%20State%20Aging%20Profile%202016.pdf
Osborn R, Moulds D, Schneider EC, Doty MM, Squires D, Sarnak DO. Primary Care Physicians In Ten Countries Report Challenges Caring For Patients With Complex Health Needs. Health affairs (Project Hope). 2015 Dec [accessed 2020 Feb 21]. https://www.ncbi.nlm.nih.gov/pubmed/26643631
Ridge PG, Hoyt KB, Boehme K, Mukherjee S, Crane PK, Haines JL, Mayeux R, Farrer LA, Pericak-Vance MA, Schellenberg GD, et al. Assessment of the genetic variance of late-onset Alzheimer’s disease. Neurobiology of Aging. 2016 Mar 3 [accessed 2020 Jan 15]. https://www.sciencedirect.com/science/article/pii/S0197458016001834